Blogs

Over the years, Malawi has grappled with allocating sufficient resources to its health sector. However, the 2024/25 fiscal year marks a significant shift as the government allocates a substantial portion of its budget to health, prioritising it over agriculture and education for the first time in history. This increase signifies a positive step towards recognising the pivotal role of health in socio-economic development.
To realise universal health coverage (UHC) and Sustainable Development Goal (SDG) 3, adequate health financing plays a crucial role in ensuring affordable, equitable and accessible healthcare. Besides SDG 3, Malawi strives to meet various health targets, including the Abuja Declaration and African Leadership Meeting (ALM)[1]commitments owing to its huge underlying health needs. For instance, the country faces significant disease burdens and poor health indicators, such as high under-5 mortality of 37.8 compared to Southern African Development Community (SADC) average of 50 deaths per 1,000 live births; maternal mortality rates of 349 compared to SADC average of 297.8 deaths; and high fertility of 4.2 children per woman against a normal rate of 2.1%.
Malawi’s health financing heavily relies on external partners, at 55% of total health expenditure, with public spending stagnant at 24% of total health expenditure and private health spending stands at 21% of total health expenditure. Previous studies in Malawi have linked slow progress in health to partly level of resources allocated to health[2]. Therefore, more funding for health is essential to address these challenges and improve healthcare outcomes in the country.
This article delves into the dynamics of health budget allocation in Malawi in 2024/2025 budget, provide a trend analysis of the investment in the health sector, what the increase means to provision of healthcare and provide recommendations to guarantee more for health for the money for Malawians.
Trends in health budget allocation
As demonstrated by Figure 1, there has been a positive trend of increasing health budget allocations over the years, indicating a growing prioritisation of healthcare in Malawi. Particularly, there’s a notable surge in the health budget allocation from 8.8% in 2023/24 to 12% in 2024/25. In the year, the health sector was allocated MK723 billion, which includes both Health and WASH (Water, Sanitation, and Hygiene). This is a substantial increase from the MK330 billion allocated in 2023/24. The health sector’s budget, excluding WASH, stands at MK554 billion, which is a 44% rise from the 2023/24 budget. This emphasises the prioritisation of healthcare as a top concern in the overall national budget.
Figure 1: Health sector allocation as a percentage of the national budget
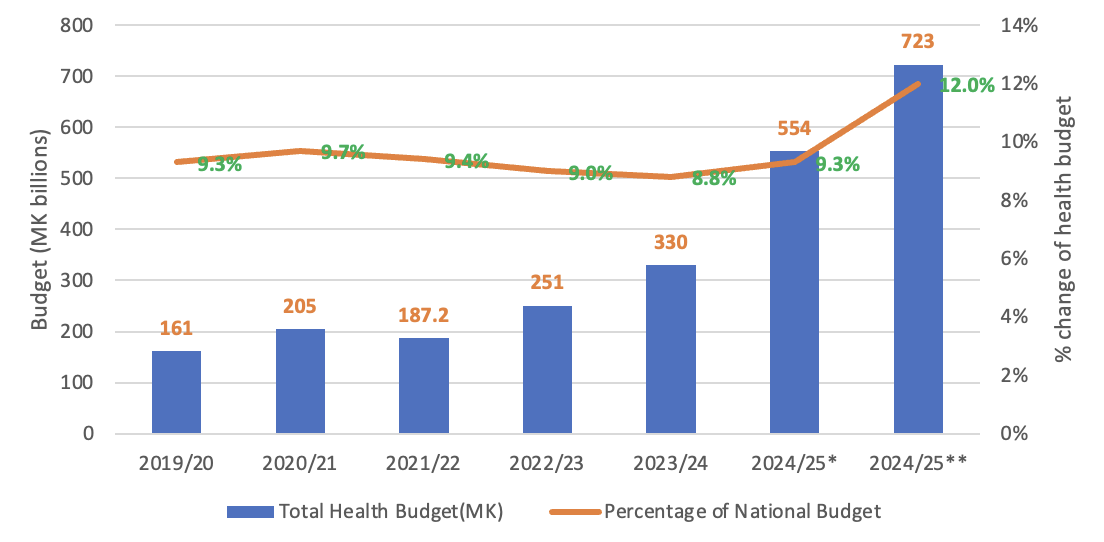
Source: Calculation from Ministry of Finance Budget figures, 2019-25
Main drivers of health sector budget allocations
The health sector budget has two parts: Ministry of Health (MoH) headquarters covering the headquarters, central hospitals and health zone offices (Figure 2), and district health covering the district hospitals and primary health services (Figure 3).
The MoH allocates funds to purchase various health goods and services, including personnel emoluments, covering salaries and benefits for healthcare workers, as well as expenses for other recurrent transactions (ORT) such as medical supplies and maintenance. Furthermore, funds are allocated for development projects, with some supported by donors and others led by the government, aimed at enhancing healthcare infrastructure and services in health facilities.
However, there are budget allocation disparities between central and district levels. The MoH Headquarters Budget saw a 79% increase, contributing significantly to the overall rise, while the District Health Services budget saw a 10% increase. It should be noted, however, that portion of the MoH Headquarters budget although managed centrally is allocated to district and primary health care levels during actual implementation (Figure 4).
Specifically, the Development Part 1 budget, which is centrally managed but allocations cater for all levels of care (including PHC), notably rose by 249%, mainly covering on-budget donor-funded projects. Medicines and Health Facilities Rehabilitation witnessed substantial increases at the district level (14% and 47% respectively). Other Recurrent Transactions (ORT) increased by 37% at the central level and 15% at the district level.
Despite the overall budget increases, there are a couple of areas of concern. Firstly, the Development Part 2 allocations, which support infrastructure across all health facilities, dropped by 38% at the central level. Secondly, the human resources budget remained unchanged despite high vacancy rates, standing at 55%, posing challenges to staffing levels in the healthcare sector. Lastly, the significant budget increase is partly due to the contribution of 34% on-budget support by development partners. After removing donor-funded supports, the overall domestic health budget only experienced a 10% increase, which is low considering high inflation rates and unfavourable foreign exchange rates. Nevertheless, when you consider domestic resource contribution levels across the three most allocated sectors (health, education, and agriculture), health allocation remains a top priority.
Figure 2: Main drivers of 2024/25 health budget allocation at central level, MK (billions)
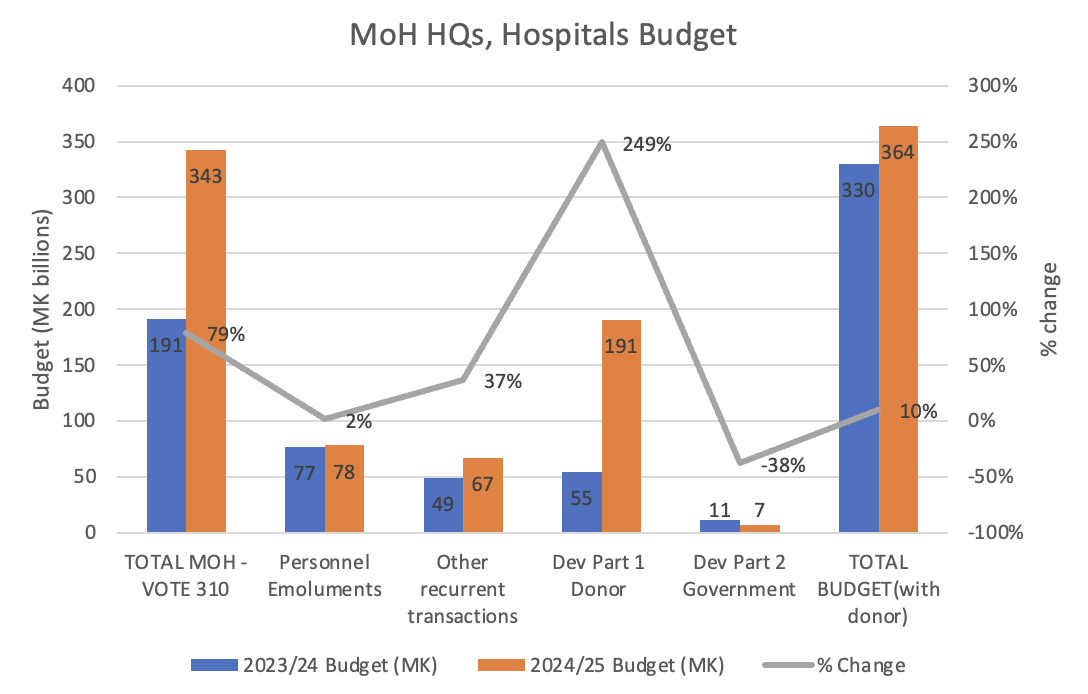
Source: Ministry of Health Budgets, 2023-25
Figure 3: Main drivers of 2024/25 health budget increase at district Level, MK (billions)
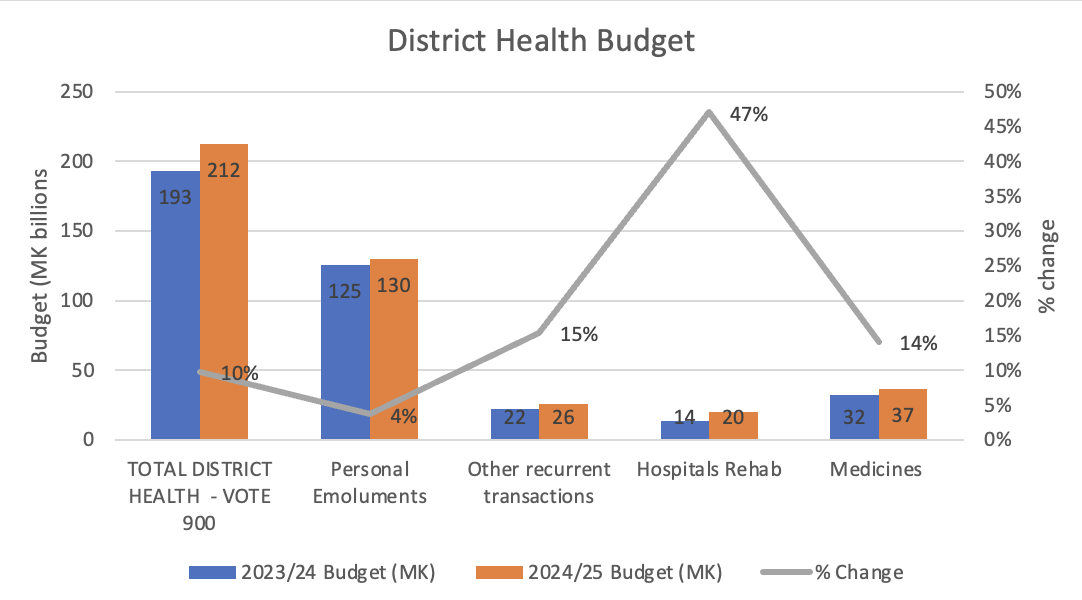
Source: Calculation from Ministry of Health Budgets, 2023-25
Investments in PHC have increased, partly due to donor support
The 2024/25 budget analysis show that primary healthcare (PHC)[1] budget allocation increased from 36.2% in 2022/23 to 41.4% in 2024/25 as a percentage of district budget (Figure 3). The allocation is aligned with the reality of Malawi’s disease burden and key health determinants are largely influenced by the performance of its PHC system[2],[3].
However, the caveat lies in the fact that allocations at PHC heavily benefited from donor support and less from the domestic resources. Evidence indicates that government funding, supported by public resources, is crucial for achieving effective coverage and financial protection compared to other funding sources. Hence, it is essential for the government to prioritise increasing funding for the health sector[4].
Figure 4: Estimate of Primary health care allocations, MK billions
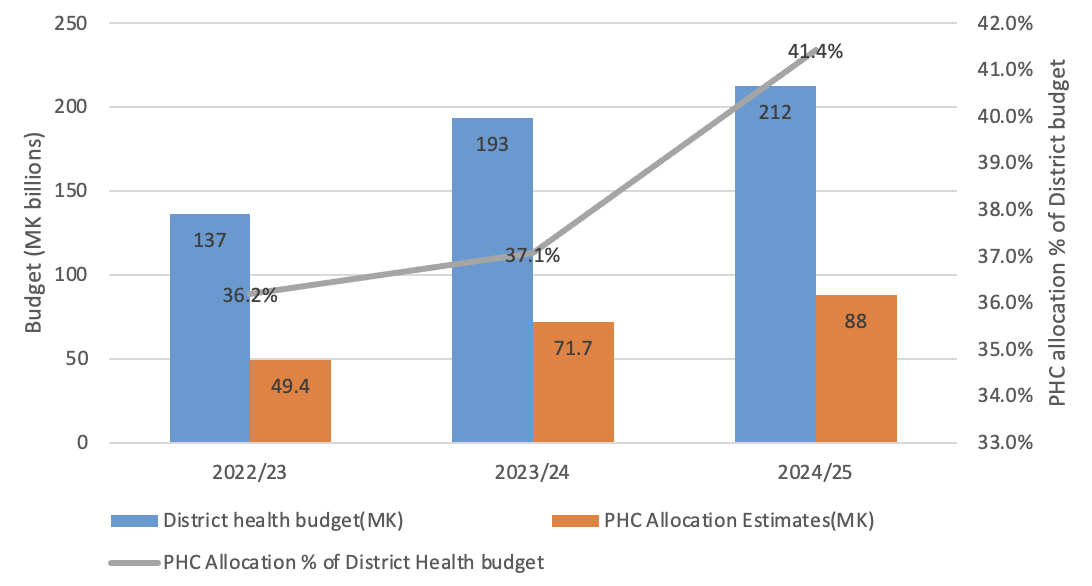
Source: Calculation from Ministry of Health Budgets, 2023-25
Impact of increased allocation on health outcomes
The overall increased allocation to health presents an opportunity to accelerate progress in health outcomes in Malawi. The increase in funding for district health services suggests a focus on strengthening primary healthcare delivery and health services at the grassroots level. The notable increases in allocations for medicines and health facilities rehabilitation at the district level signify efforts to enhance access to essential medicines and improve the quality and functionality of health facilities at the local level.
The increase in ORT both at Central and District levels will support the smooth functioning of health systems, ensure the availability of essential resources for service delivery, and contribute to the sustainability of health programs and operations.
How to optimise the impact of budget allocation
While the increase in funding offers the opportunity to expedite progress in health outcomes in Malawi, it also poses risks and challenges in ensuring that the resources lead to fair and sustainable enhancements. To garner more health benefits from this budget, it is crucial to address inefficiencies and wastage within the healthcare system that hinder the efficient utilisation of resources.
The health financing strategy highlights several areas with potential for generating savings, including in-service training, supply chain management, prevention of medicines and medical supplies pilferage, infrastructure contract management, and addressing fragmented data systems. Therefore, concerted efforts must be focused on combating corruption, improving public financial management systems, and enforcing rigorous accountability mechanisms to minimise wastage and ensure prudent utilisation of resources.
In addition, the Malawi government should redirect more public funds (domestic resources) towards primary healthcare. By allocating a greater portion of the budget to primary healthcare, the government can prioritise preventive and promotive healthcare measures, ultimately reducing the burden of preventable diseases and improving overall health outcomes.
Also, the government should diversify domestic revenue sources to reduce its reliance on donor funding, thereby ensuring a more stable and sustainable revenue stream for healthcare. Significantly, the government should prioritise investments in critical gaps including health infrastructure and workforce capacity, crucial for strengthening the healthcare system, and reduce inefficiencies in various areas of the healthcare system.
Finally, the rise in the overall health budget can be attributed to the efforts of various stakeholders, including Members of Parliament, civil society, the Ministry of Health, development partners, and notably, the political commitment of the Malawi government. This highlights the effectiveness of coordinated advocacy, political determination, and engagement with stakeholders in fostering beneficial outcomes. Looking ahead, it is crucial to maintain this momentum, capitalise on achievements, and establish comprehensive monitoring and evaluation systems to monitor progress and tackle evolving obstacles efficiently.
Conclusion
The significant increase in health budget allocation underscores a positive stride towards prioritising the health and well-being of Malawian citizens. However, sustained efforts are required to address donor dependency, inefficiencies, and wastages within the healthcare system to realise maximum impact and ensure equitable and sustainable improvements in health outcomes. Collective advocacy, political will, and stakeholder engagement will be instrumental in driving positive change and achieving the desired health goals in Malawi.
References
[1] In February 2019 the Heads of State and Government endorsed the outcomes of the Africa Leadership Meeting (ALM) and adopted declarations in support of mobilising greater domestic resources for health in Africa
[2] McGuire F, et al. (2020). Allocating resources to support universal health coverage: development of a geographical funding formula in Malawi. BMJ Global Health. doi:10.1136/bmjgh-2020-002763
[3] Calculations are based on WHO Accounting measure for PHC and Malawi NHA distribution ratios (Measuring primary health care expenditure under SHA 2011: technical note, December 2021. Geneva: World Health Organization; 2022)
[4] Malawi Demographic and Health Survey 2015-16
[5] Makwero M.T. (2018). Delivery of primary health care in Malawi. Afr J Prm Health Care Fam Med. https://doi.org/10.4102/ phcfm.v10i1.1799
[6] Xu, K., A. Soucat, J. Kutzin, C. Brindley, N.V. Maele, et al. (2018). Public Spending on Health: A Closer Look at Global Trends. Geneva: World Health Organization

