Blogs
The persistent rise in health expenditures, coupled with fiscal pressures, has prompted widespread calls for efficiency improvements within healthcare systems. However, tackling the root causes of inefficiencies remains a significant challenge. Effective utilisation of data is essential for pinpointing and addressing inefficiencies in healthcare budgeting and expenditure.
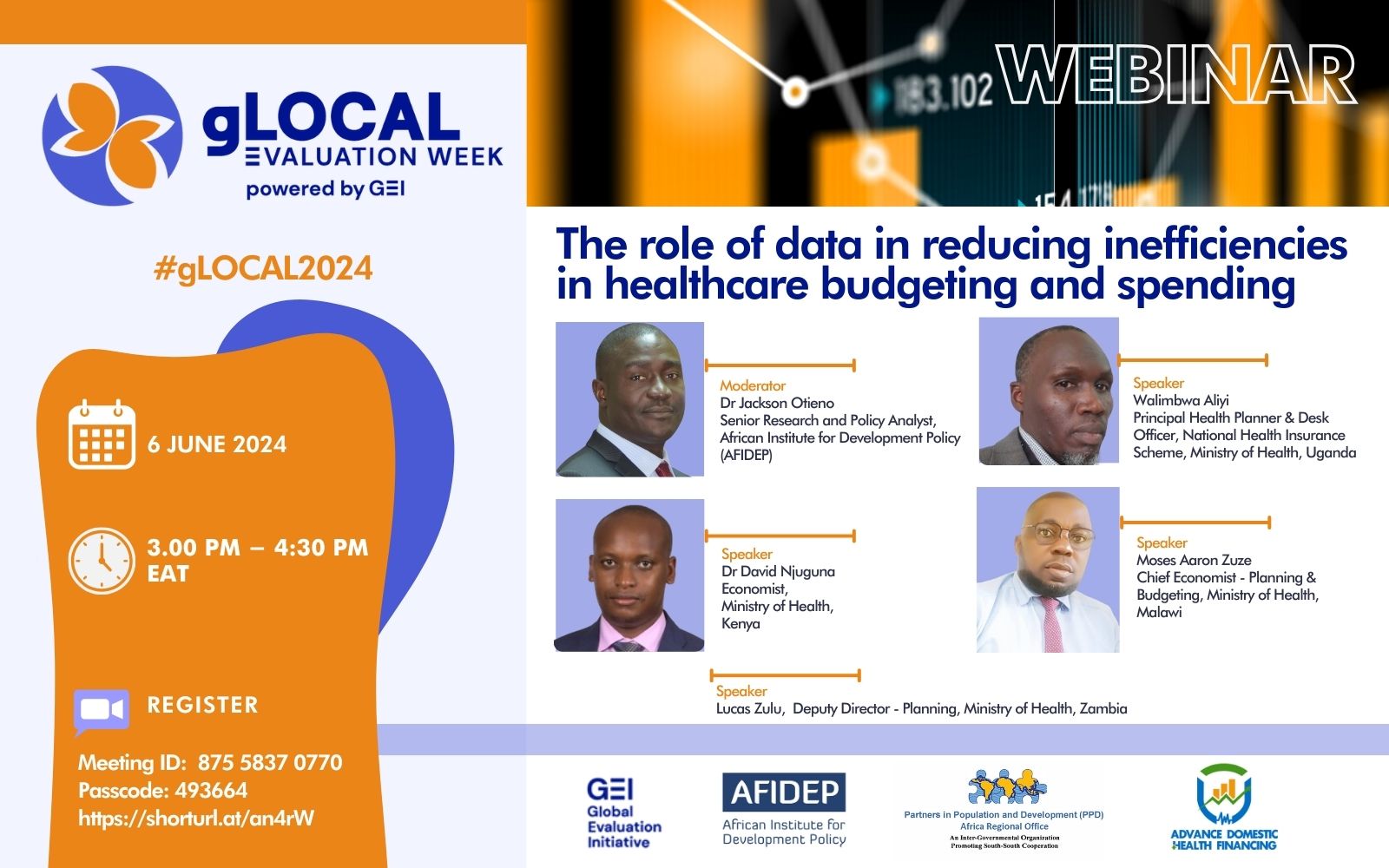
This challenge of healthcare systems, particularly in Africa, was addressed during a webinar organised by the African Institute for Development Policy (AFIDEP) and Partners in Population and Development – Africa Regional Office (PPD-ARO), as part of the Advance Domestic Health Financing (ADHF) project. The project works with the governments of Zambia, Kenya, Malawi and Uganda to enhance domestic investments in healthcare and promote efficient utilisation of healthcare budgets, focusing on primary healthcare (PHC), girls’ and women’s health.
During the webinar held during the gLOCAL Evaluation Week, officials from Ministries of Health (MoHs) in Kenya, Uganda, Zambia, and Malawi, shared valuable insights and country-specific experiences on leveraging data to address inefficiencies in health budget allocation and spending.
Key insights and highlights from Kenya
In Kenya, the government has used various key sources of data such as National Health Accounts, Public Expenditure Reviews, Out-of-Pocket Estimation, and Public Expenditure Tracking Survey to address inefficiencies in healthcare. The insights gathered from these sources have been instrumental in guiding the government on actions needed to achieve universal health coverage (UHC). This has included greater resources put towards primary healthcare (PHC). Thus, expenditures related to PHC have significantly increased in recent years. Between the fiscal years 2016/17 and 2020/21, PHC spending increased from KShs 245.23 billion to KShs 284.91 billion.
The Public Expenditure Tracking Survey has played a crucial role in identifying leaks within the healthcare system. This has prompted the introduction of the Public Funding Financial Management Act, which provides guidelines on the proper utilisation of healthcare resources from the Exchequer to health facilities. This initiative aims to reduce bureaucratic hurdles and prevent resource wastage due to corruption.
Furthermore, the adoption of the Integrated Financial Management Information System (IFMIS) within the commodity supply system has significantly enhanced stock management and minimised wastage. IFMIS facilitates real-time ordering and management of stocks, thereby improving the efficiency of requisitions and stock replenishment processes.
Key insights and highlights from Uganda
In Uganda, several key sources of data play crucial roles in shaping health policy and resource allocation decisions. The National Health Accounts (NHA) track trends in domestic financing for health sub-programmes. For the last seven years (2017/18–2022/23), NHA has recorded a rise in healthcare investment from UGX 1.827 trillion to UGX 3.685 trillion. This includes increased funding for medicines from UGX 396.17 billion to UGX 513 billion between 2019 and 2023. Also, NHA has recorded a strategic shift towards prioritising financing PHC over curative services, exemplified by the PHC grant increasing from UGX 625.18 billion to GX 1,008.1 billion from 2020/21 to 2023/24.
The Health Management Information System also provides critical data on disease conditions, demographics, and poverty metrics, guiding equitable resource allocation and programme implementation. Overall, these data-driven approaches support Uganda’s health sector in optimising funding efficiency, enhancing service delivery, and addressing public health challenges effectively.
Key insights and highlights from Malawi
In Malawi, efficient data utilisation has led to positive changes such as a notable rise in health budget allocation, prioritisation of PHC to prevent diseases, fraud prevention through IFMIS generated local purchase order, improved monitoring and evaluation, and the establishment of Direct Facility Financing (DFF) guidelines for fair resource distribution among districts.
The DFF focuses specifically on an intra-district resource allocation formula to govern the distribution of health resources among community hospitals and health centres within each district. By setting clear budget targets, monitoring expenditures, and evaluating the impact of healthcare investments under a unified framework of “one budget, one plan, and one M&E,” the MoH seeks to strengthen budgeting processes.
Key insights and highlights from Zambia
Zambia’s healthcare system has adopted a data-driven approach to enhance efficiency. By utilising systems like the IFMIS and the Electronic Logistics Management Information System (eLMIS), Zambia tracks healthcare expenditures and manages medical supplies effectively.
The country applies data to enhance transparency in the use of healthcare resources, supply chain optimisation through real-time data on stock levels, and monitoring and evaluation to identify and eliminate inefficiencies like discrepancies in billing practices, and medication or service provision usage. Despite challenges such as data quality, inadequate internet connectivity, and insufficient ICT resources, Zambia is committed to improving data utilisation for strategic planning and resource allocation in the health sector.
Conclusion
The webinar emphasised the indispensable role of data in reducing inefficiencies in healthcare budgeting and spending across different African countries. Each country’s experience underscored the need for robust data systems, strategic planning, and evidence-based decision-making to optimise health outcomes and resource utilisation. The insights shared serve as a blueprint for other countries aiming to strengthen their healthcare systems through effective data integration.
Watch the webinar here: https://youtu.be/wSOlsAitSws

