Research Briefs
The global clean energy transition is essential for climate resilience but risks worsening gender inequality if women are excluded from its design and benefits. In Africa, women’s limited access to capital, technical training, and decision-making opportunities hinders their participation in the energy sector. A review of studies and interviews highlights both these challenges and successful models like Solar Sister, which show the impact of women-led initiatives. The brief recommends increasing women’s roles in energy governance, investing in financial and Science, Technology, Engineering, and Mathematics (STEM) education, and creating tailored financing for women entrepreneurs to ensure an equitable and inclusive energy […]
Gender-based violence (GBV) remains a serious public health, human rights, and socio-economic issue in Kenya despite strong legal and policy frameworks. Survivors continue to face stigma, fear, weak law enforcement, and limited access to justice and support services. A targeted literature review of 34 studies (with 9 meeting inclusion criteria) found persistent service gaps but also identified promising interventions such as multi-sectoral coordination, stronger forensic systems, survivor centered economic empowerment, community-based mental health support, and digital tools for protection. The evidence brief calls for a coordinated, survivor centered, and multi-sectoral approach that integrates health, legal, economic, psychosocial, and technological responses […]
AI has the potential to transform energy access in low- and middle-income countries by improving affordability, reliability, and efficiency through innovations like predictive maintenance, smart metering, and energy forecasting. These tools support decentralised renewable energy systems, especially in off-grid areas. However, without inclusive design and governance, AI risks reinforcing existing gender and social inequalities. To ensure equitable energy transitions, governments and development partners must prioritise gender-responsive design, build local technical capacity, and establish strong ethical governance frameworks. Read more:
Public Accountability Committees (PACs) in Africa play a crucial role in governance, but they face significant challenges, including limited independence and insufficient resources, weak legal mandates, and low public engagement. Drawing on a thematic review of 30 studies and key stakeholder consultations, this evidence brief outlines reform priorities, including strengthening legal frameworks, boosting resource allocations, integrating advanced technology, and enhancing public engagement. Implementing these recommendations can significantly enhance transparency, accountability, and public trust across African governance systems, thereby improving PACs operation. Read more:
Kenya’s arid and semi-arid lands (ASALs), which comprise over 89% of the country’s landmass, are increasingly affected by climate change-induced droughts, erratic rainfall, and environmental degradation. These regions, home to millions of Kenyans who rely on pastoralism and rain-fed agriculture, face heightened food insecurity and disruptions to their livelihoods. This policy brief synthesises recent research and proposes strategic recommendations to enhance food security and resilience in these vulnerable areas. It emphasises the need for an integrated policy framework that mainstreams climate resilience, promotes gender inclusivity, invests in sustainable land and water management, and strengthens early warning and social protection systems. […]

This story of change is part of a series that illustrates the early results of a 2-Week Virtual LEEPS Evidence-Informed and Equity in Policymaking Training Workshop delivered to members of the Africa Research Impact Network (ARIN) who attended the training. The stories of change illustrate how the training has improved the training of researchers in higher learning institutions, grant writing, advocacy strategies, research into policy and practice processes and project/ programme design and implementation. Download:

This parliamentary briefing provides an overview of the TB burden in Africa, highlighting the disproportionate burden on men and the broader impact on communities. It outlines actionable recommendations for policymakers, focusing on gender-responsive TB policies, increased awareness, strengthened partnerships, and sustainable funding to enhance equitable access to TB prevention, diagnosis, and treatment. Download to read more:
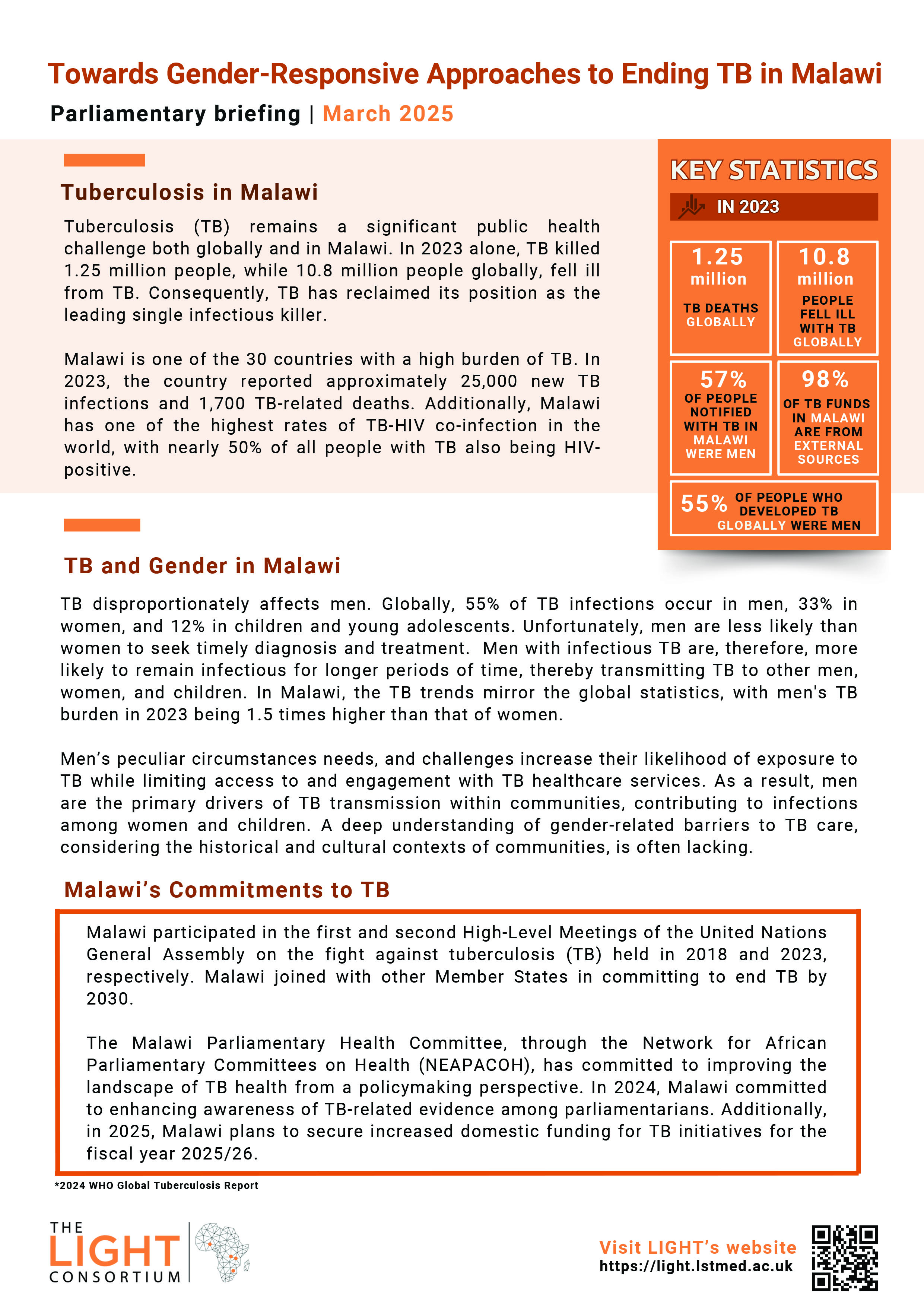
This parliamentary briefing provides an overview of the TB burden in Malawi, highlighting how TB disproportionately affects men, Malawi’s commitments to TB, the policy landscape, the funding challenges for TB and LIGHT Consortium’s key asks for the parliamentarians. Download to read more:

This parliamentary briefing provides an overview of the TB burden in Africa, highlighting the disproportionate burden on men and the broader impact on communities. It outlines actionable recommendations for policymakers, focusing on gender-responsive TB policies, increased awareness, strengthened partnerships, and sustainable funding to enhance equitable access to TB prevention, diagnosis, and treatment. Read more:
From 2017 to 2020, Rwanda’s current Gross Domestic Product (GDP) showed a positive trend, rising from 882 billion USD to 919 billion USD in 2019-20. Over the same period, regarding healthcare financing, Rwanda’s Total Health Expenditure (THE) witnessed a steady increase over the three years under review. Additionally, THE as a percentage of GDP also demonstrated an upward trajectory, reflecting the country’s commitment to healthcare investment. Furthermore, Rwanda’s per capita THE in USD exhibited an upward trend over the same period. Download the evidence brief to read more on the findings.
Despite successes, challenges remain in extending coverage to informal sector workers and addressing disparities in service accessibility across regions. The review of Indonesia’s health financing approaches provides valuable insights for other countries, particularly in leveraging private sector participation, enhancing revenue and risk pooling, and decentralising health spending to improve service delivery.

Zambia has made some progress in improving its health system and expanding access to health services, especially for the poor and vulnerable groups (Masiye et al., 2016). However, it still relies on external funding, high out-of-pocket (OOP) payments, and low coverage of health insurance (Chansa et al., 2020). To address these challenges, Zambia has adopted and implemented various innovative health financing mechanisms. This evidence brief unpacks the health financing mechanisms in Zambia.

