Blogs

“Reducing global mortality from infectious diseases, especially in fragile populations, builds upon our progress in preventing and treating sepsis effectively” Dr Tedros Adhanom Ghebreyesus, Director-General, World Health Organisation (WHO), ‘Global Burden of Disease Report,’ 2020.
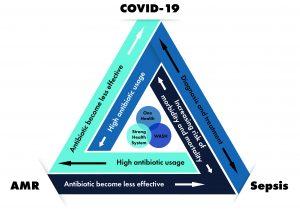
What lessons can stakeholders in Africa who are concerned about sepsis and antimicrobial resistance (AMR) learn from COVID-19? Sepsis is a life-threatening condition caused by the body’s toxic response to infection that frequently results in death or serious disability. Globally, sepsis is the second biggest cause of death and the leading cause of preventable death. With high rates of infection, Africa is expected to be greatly affected by sepsis. Despite its massive death toll, sepsis remains widely unknown and under-prioritised by the general public, health care workers, and decision-makers. Awareness of and knowledge on what sepsis is and its burden on society is critical. With the emergence of the COVID-19 pandemic, an infectious disease caused by a newly discovered coronavirus (SARS-CoV-2 virus), and the growing threat of inappropriate use of antibiotics causing antimicrobial resistance (AMR), how will this contribute to the global burden of sepsis?
AFIDEP, through the African Research Collaboration on Sepsis (ARCS) programme and Drivers of Resistance in Uganda and Malawi DRUM) consortium, is contributing to the body of scientific knowledge on sepsis and AMR.
World Sepsis Congress Spotlight
On 9 September 2020, WHO and the Global Sepsis Alliance (GSA) hosted a World Sepsis Congress Spotlight: Sepsis, Pandemics, and Antimicrobial Resistance – Global Health Threats of the 21st Century. A free online event that sought to review the achievements and challenges of potential solutions to combat the threat of sepsis worldwide. The event also served as a launch for the WHO’s report on sepsis “Global Report on the Epidemiology and Burden of Sepsis: Current Evidence, Identifying Gaps and Future Directions” dubbed “Global Burden of Disease Report.”
In developing the report, ARCS experts were part of a technical expert consultation first gathered in October 2019 in Geneva, Switzerland, in reaching consensus on the contents of the document and also providing an external review of the report.
COVID-19 and Sepsis
According to the WHO Global Burden of Disease Report, sepsis is the cause of 1 in 5 deaths worldwide and disproportionately affects vulnerable populations: men, newborns, pregnant women and people living in low-resource settings. Early studies in Wuhan, China, found sepsis to be the most frequently observed complication in COVID-19 patients. As a result, sepsis is being applied in the diagnosis of COVID-19 complications. For instance, the diagnostic criteria of sepsis and septic shock are being used as a reference for the criteria of the severity of respiratory insufficiency among COVID-19 patients. Sepsis is also a pathway to COVID-19 morbidity and mortality and is a risk factor for in-hospital COVID-19 deaths.
Understanding of the relationship between sepsis and COVID-19 is leading to the innovative treatment of COVID-19.
Sepsis and AMR
When identified early and treated timely with antibiotics, sepsis fatality risk is reduced. However, this could lead to the misuse of antibiotic usage and jeopardise clinical management of sepsis. A high level of drug resistance exists to commonly prescribed antibiotics on the African continent. According to the WHO report, AMR also contributes to the medical and economic burden of infectious diseases.
The high prevalence of sepsis demands for more antibiotic usage to address it, while the growing AMR calls for limited use of antibiotics to reduce AMR spread. While this appears to present a competing situation, there exist some positive relationships between the two. Linkages are seen on how the two (sepsis and AMR) occur and addressed collectively through a robust health system, improving hygiene in the health facilities and improving sanitation and hygiene in the communities.
AMR and COVID-19
While COVID-19 itself is a viral infection, evidence shows that it leads to secondary infections in many cases, including secondary bacterial pneumonia, as well as complications from infections such as sepsis and septic shock, that require antibiotics. There is no doubt that antibiotics are a critical tool in treating secondary infections associated with COVID-19.
Amid the pandemic, there have also been calls to uphold the principles of antimicrobial stewardship (AMS), including the preservation of antibiotics for cases with severe symptoms, microbiological tests before use of antibiotics, and recommendations for duration and type of antibiotic treatment.
Overcoming sepsis, AMR and COVID-19
The WHO report indicates that low-income countries face severe resource limitations such as personnel skills, medical facilities and policies to make their health systems functional. However, Sub-Sahara Africa has been least affected by COVID-19, and lessons can be drawn from COVID-19 to answer some questions about how a focus on sepsis and AMR can create a robust health system that effectively puts health in control. The creation of a robust health system worldwide requires the continued promotion of quality improvement. COVID-19 has taught us the importance of improved sanitation, water quality and availability, and infection prevention and control measures, such as appropriate hand hygiene, which can prevent sepsis and AMR. Finally, as COVID-19 likely spreads to humans from animals such as bats, it is critical to take a multidisciplinary One Health approach to better understand this and future infectious disease challenges.
Conclusion
Researchers need to build the scientific evidence of treating sepsis and AMR with insights from COVID-19, which have shown successful outcomes in Africa, such as those among all COVID-19-infected neonates with clinical signs of sepsis. This evidence should inform global health policymakers to support healthcare workers caring for critically ill sepsis and AMR patients.
ARCS is a Global Health Research Group awarded by the National Institute for Health Research (NIHR grant reference number 17/63/42) and led by the Liverpool School of Tropical Medicine (LSTM). This blog presents independent research funded by the NIHR. The views expressed are those of the author and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
The Drivers of Resistance in Uganda and Malawi DRUM) consortium is a project awarded by the UK Research and Innovation (UKRI) and Department of Health and Social Care (DHSC) and is managed by Medical Research Council (MRC). The views expressed are those of the author(s) and not necessarily those of the UKRI, DHSC or MRC.
Related Posts





