Blogs

The global burden of tuberculosis (TB) remains alarmingly high. Though Kenya, one of the high TB burden countries in Africa, has made significant progress in combating TB, more efforts are required to meet the 2030 End TB Strategy targets. TB, continues to be a leading cause of respiratory-related hospitalizations and deaths in Kenya.
The TB and Lung Health Symposium 2025, held on 29-30 September in Nairobi overaching theme was “Innovation and Integration in Advancing TB and Lung Health”. The event brought together a diverse group of stakeholders to reimagine respiratory care.It was hosted by the Kenya International Scientific Lung Health Conference (KISLHC) and organised by the LIGHT Consortium’s partner the Respiratory Society of Kenya (ReSoK) together with other key technical partners, Ministry of Health, The National Tuberculosis, Leprosy and Lung Disease Program (NLTD-P), Centre for Health Solutions-Kenya, AMREF Health Africa in Kenya, the African Institute for Development Policy (AFIDEP), Kenya Medical Research Institute (KEMRI), Stop TB Partnership – Kenya, Kenyatta National Hospital (KNH), Clinton Health Access Initiative (CHAI), Network of Tuberculosis Champions Kenya, QURE.AI, Glenmark, Wadhwani AI Global and MSG, all united by a shared commitment to advancing lung health in Kenya.
Here are our reflections on key TB messages delivered during the symposium.
Are we there yet?
Kenya has made significant progress in the TB cascade, from screening and diagnosis to treatment, including initiatives on post-TB lung disease. Improvements include 75% TB treatment coverage, better TB detection rates, the adoption of AI-powered diagnostic tools and digital Chest X-rays, molecular WHO-recommended rapid diagnostic tests, updated childhood TB algorithms, shorter regimens for children and Drug Resistant TB management, as well as a focus on research to guide implementation.
The National Strategic Plan (NSP) 2023/24–2027/28 aims to eliminate TB deaths and suffering by 2030.
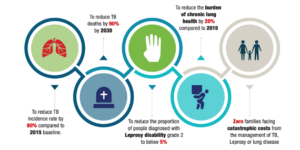
Figure 2: National Strategic Plan for TB, Leprosy and Lung Diseases, Kenya2023/24–2027/28
The recently concluded 2024 Drug Resistant TB survey demonstrated a decline in prevalence rates. Despite a 41% drop in overall TB incidence and a 66% reduction in deaths since 2015, these figures fall short of the 2025 End TB targets of 50% and 75%. The 2022 Nairobi TB Prevalence Survey found a persistently high TB rate of approximately 806 cases per 100,000 people, with no significant decline since 2015. TB prevalence among men remained high at 1301/100,000, and the age group with the highest prevalence was 45-54 years. Persistent challenges like funding, treatment gaps, and inequities in care access, especially among vulnerable populations continue to slow the progress.
What must we do to END TB?
The symposium speakers had interesting perspectives on what we must do as a country to end TB.
Address social determinants of health
“Ending TB, is not just a medical challenge—it’s a political and social imperative. The conditions in which people are born, grow, live, work, and age influence health risks and outcomes, directly impacting TB transmission, progression, and care.”
Prof. Jeremiah Chakaya, Chief Executive Officer of ReSoK
Kenya cannot meet its End TB targets without addressing systemic issues like poverty, poor housing, food insecurity, limited education, and climate change.Drawing lessons from historical TB declines in England, Wales and screening interventions in Indonesia, Prof. Chakaya noted that biomedical tools alone are insufficient. A dual approach is required, addressing structural inequities as well as biomedical interventions. For example, deploying advanced diagnostics while investing in social interventions that guarantee decent living conditions, education, and protection from inequality. Dr Nkirote Mugambi-Nyaboga from Centre for Health Solutions-Kenya also highlighted the need to focus on nutrition as prevention.
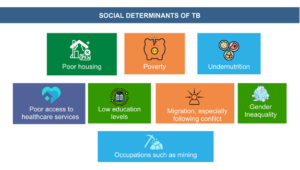
Figure 3: Source Respiratory Society of Kenya
offer person-centred tb care, addressing gender and age in programming
Mr Aiban Ronoh (Head Monitoring and Evaluation and Research) and Dr Jane Ong`ang`o (Principal Research Scientist, KEMRI) highlighted that men continue to be most affected by TB, additionally, they noted an increasing prevalence in older age groups as an emerging group at high risk of TB.
Dr Brenda Mungai, Research Uptake Lead at AFIDEP under LIGHT consortium highlighted the WHO`s recent policy brief on Tuberculosis among populations at high risk and people in vulnerable situations’ . The brief highlights the importance of identifying individuals and populations at higher risk for TB for effective planning, resource allocation, optimal and equitable delivery of people-centred, human rights-based TB services.
LIGHT Consortium research findings across Kenya, Uganda, Nigeria, and Malawi reveal that TB disproportionately affects men, with gender dynamics influencing access and outcomes for all. A modelling study by LIGHT indicates that increasing treatment coverage among men and addressing structural risk factors could reduce overall TB incidence by up to 25%, benefiting women and children as well.
Adolescents and young people are particularly underserved, often falling through the cracks of adult-focused systems. Rhoda Pola, an Early Career Researcher at ReSoK also shared LIGHT study insights and evidence on the experiences of adolescents and young adults acessing TB services in Kenya, showing long diagnostic pathways, stigma, and structural barriers.
Offering person-centred TB care that addresses gender and age considerations ensures the unique needs of different populations are met, leading to more effective and equitable services. Nationally, stakeholders must raise awareness of gender disparities, promote multisectoral collaboration, and engage communities in shaping inclusive, stigma-free policies. At the facility and county levels, priorities include strengthening health information systems to collect and use sex-disaggregated data, training frontline workers in gender-responsive care, and documenting best practices.LIGHT advocates for youth-friendly services with welcoming clinics, flexible hours, and faster service. Health workers should communicate effectively and offer counselling that addresses fears and misconceptions. Awareness campaigns must be tailored to gender-specific beliefs and delivered through platforms young people use.
For the emerging high risk group of older adults, TB care should include early detection, age-specific guidelines, integration with elder care systems, and increased provider awareness. By centering gender and age, TB care becomes more equitable and responsive to real-world needs.
adopt Innovations, research and integration of services
A future built on Innovation, Integration, and ownership
Dr Immaculate Kathure, Head of the National Tuberculosis, Leprosy, and Lung Disease, emphasized the role of innovations in delivering quality TB and lung disease care. Kenya, a front runner in adopting innovations, will pilot near point-of-care diagnostic tests, as highlighted by Dr Enos Masini Senior Disease Advisor TB, Global Fund. This initiative aims to close diagnostic gaps and accelerate treatment initiation, especially in underserved areas. Early adopter countries will generate operational evidence, validate implementation models, and shape policy pathways for scale-up. Dr Videlis Nduba, National Principal Investigator KEMRI, shared promising progress in the Phase 3 clinical trial for the M72/AS01E TB vaccine, potentially the first new TB vaccine in over 100 years.
As global funding for TB declines, Kenya must prioritise domestic investment, innovative financing, resource optimisation and multisectoral engagement. Dr Salome Okutoyi, Deputy Centre of Excellence Director, US Department of State, emphasised the importance of country-led domestic co-financing, integrated into national systems and policies. County assemblies, especially health and budget committees, play a critical role in closing funding gaps, with localised TB data helping to justify resource allocation and demonstrate urgency. The private sector remains an underutilised partner. Models like India’s “Adopt-a-Patient” initiative offer inspiration, whether through food support, direct funding, or community-driven care. Everyone has a role to play in sustaining Kenya’s TB response.
Kenya’s TB response is increasingly research-driven. Mr Rono highlighted that the national task force is coordinating studies on vulnerable populations, digital diagnostics, patient costs, and lung disease burden. These efforts aim to inform policy and improve service delivery, with bi-annual dissemination meetings ensuring evidence translates into action.
Integration of TB into essential health service packages, leads to aligned resources, defined coverage, and strengthening of entire health system. Tuberculosis and primary health care policy brief guides countries in exploring the synergies between the PHC approach and the TB response and underscores the role of multisectoral action and empowered communities.
Conclusion
The TB and Lung Health Symposium 2025 was a transformative event, positioning Kenya to lead in redefining respiratory care through innovation, integration, and ownership. The fight against TB must be inclusive, equitable, and evidence based.
The LIGHT Consortium is at the forefront, focusing on gender in TB care. Their research across Kenya, Uganda, Nigeria, and Malawi reveals how gender norms affect access, diagnosis, and treatment outcomes, translating these insights into actionable policy recommendations. As Kenya and its partners advance, LIGHT’s evidence and leadership will be crucial to ensure no one is left behind.

