News
Emerging evidence shows that a large proportion of healthcare financing in Kenya is “out-of-pocket’. This means that Kenyans bear the highest costs of accessing health services, which often result in catastrophic effects on the livelihoods of the majority poor.
According to Mr. Thomas Maina, Senior Health Financing Advisor at Health Policy Plus, a USAID-funded programme, when households invest a lot of their resources in healthcare, the country risks increasing poverty levels among the population.
Speaking at a policy dialogue hosted by the Parliament of Kenya in collaboration with AFIDEP, Mr Maina highlighted key health financing issues that need to be addressed in order for Kenya to achieve universal health coverage (UHC). According to the World Health Organization (WHO), UHC is a state of health governance where everyone, everywhere, can access quality health services without being forced into poverty.
The meeting noted that Kenya could learn from other countries like Indonesia, Thailand and Mexico, that have made good strides in enabling UHC. A World Bank representative, Dr. Njeri Mwaura, indicated that some of the lessons that Kenya could learn from these countries include focusing health financing and other efforts on the greatest contributors to the country’s burden of disease and the most vulnerable sections of the Kenyan population.
Financing UHC is a key obstacle that Kenya must overcome in order to achieve the third Sustainable Development Goal (SDG 3) goal of ensuring healthy lives and promoting well-being for all, which aligns well with Kenya’s Vision 2030.
The country’s National Hospital Insurance Fund (NHIF) is the government’s main insurance fund for covering healthcare costs for Kenyans. Although the fund’s Acting CEO Mr. Geoffrey Mwangi said that the fund has been highly successful in expanding accessibility to healthcare across the country, the fact that the fund still does not cover all Kenyans shows that there is still a long way to go for this fund to enable UHC. Notably, the fund only covers those who have the ability to make monthly financial contributions, and leaves out all those who lack the ability to make such contributions. It is, however, commendable that the NHIF has expanded the list of services to include kidney dialysis and some range of range of cancer treatments, as reported by Mr Mwangi. Further, the fact that informal sector workers only contribute to the fund on a voluntary basis means the NHIF kitty is not as large as it would be if contribution were compulsory, as is the case with those in formal employment. “These resources (from the informal sector) can drive the country towards achievement of universal health coverage,” noted Mr Mwangi.
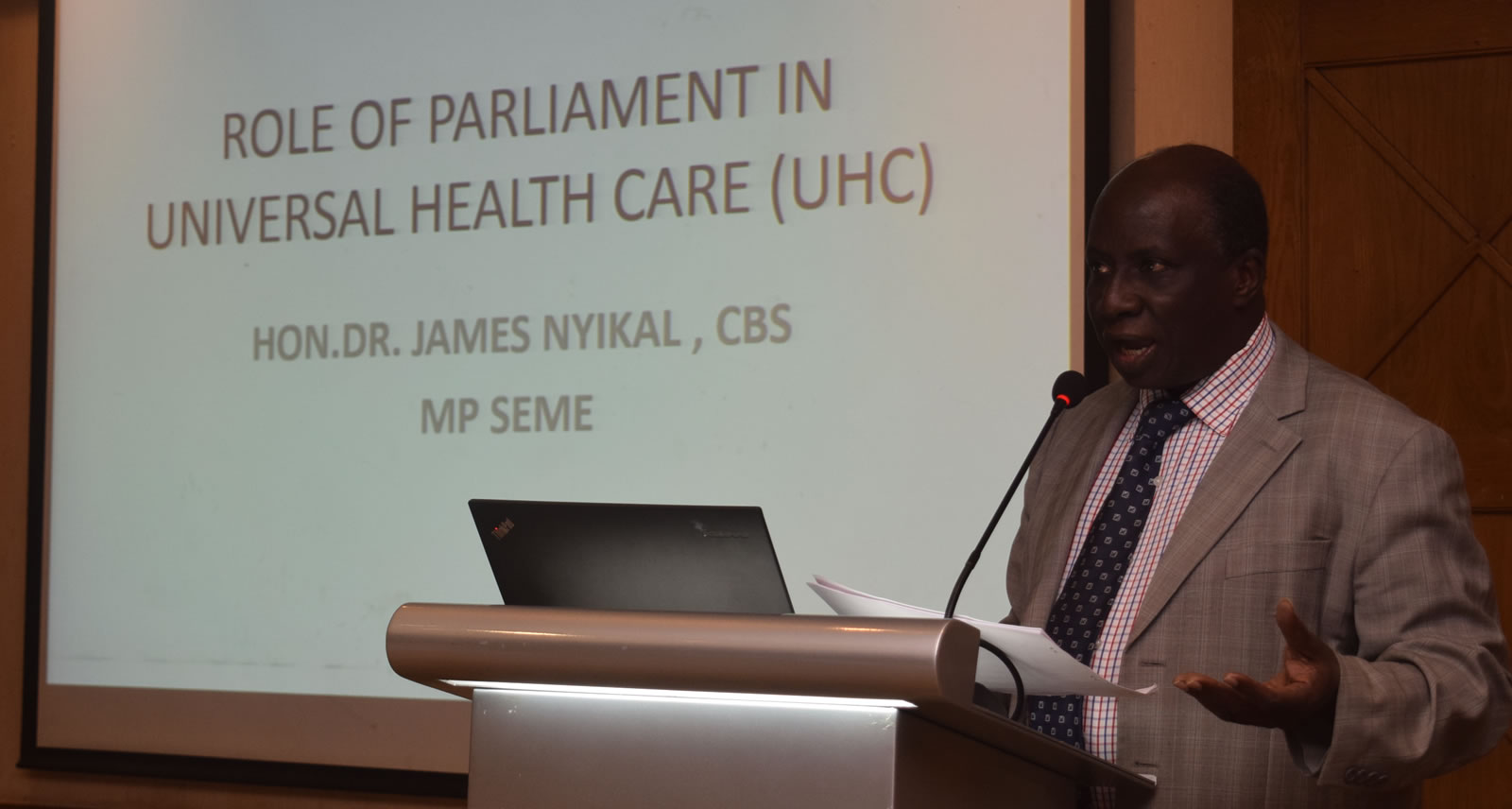
The meeting deliberated the role of Parliament in making UHC a reality in Kenya and not a mere “goal on paper.’ Hon. Dr. James Nyikal, the MP for Seme and Chairperson of the UHC sub-Committee of the National Assembly, noted that it is time the country implemented the lessons learned from countries that have achieved this goal. Hon. Nyikal reiterated that Parliament has an advocacy role to play, coupled with providing a legal framework for implementation of UHC. Specifically, the Kenya Health Bill proposes an overarching framework for implementation of UHC. This is complemented by regulatory laws such as those concerned with regulation of the quality of human resources in the health sector, products and equipment, and healthcare institutions.
In addition, Hon. Nyikal noted that stakeholders need to collaborate with the relevant Parliamentary Committees in order for the country to actualise UHC. Speaking on behalf of the Parliamentary Health Committee which she chairs, Hon Rachael Nyamai indicated the Committee would devote itself to ensuring UHC is achieved in Kenya.
Urgently increase health sector budget
Having engaged exhaustively on the opportunities and challenges for Kenya to achieve UHC, various recommendations emerged. With health financing emerging as one of the major obstacles, it is of paramount importance that the government adopts innovative mechanisms to mobilise adequate financial resources in a sustainable and efficient manner. This is with the goal to ensure access to essential health services without exposing Kenyans to financial hardship. With resources from donors being on the decline, this is a step the government needs to take urgently.
Address key health system challenges “ human resources, health facilities
There is also need for adequate human resources as the country is in short supply of qualified health workers. Further, equal distribution of well-equipped health facilities and a functioning health information system (HIS) are critical investments.
Strengthen public private partnerships in healthcare provision
Public-private partnerships (PPPs) are no new concept to Kenya’s development agenda. However, this needs to be central to the implementation strategy for UHC in the country. As stated by Dr. Amit Thakker, the Chairman, Kenya Healthcare Federation, 90 percent of corporates in Kenya contribute to the healthcare of their staff and families through health insurance. However, he noted that although one in 20 Kenyans have a strong health insurance cover, 16 out of 20 have no cover, and this is where key investments should be made. Parliamentarians were also challenged to ensure a policy framework that encourages PPP so healthcare in Kenya can benefit from the synergies of both government and the private sector.
Dr. Thakker further challenged the government’s focus on one pool of resources (i.e. NHIF), arguing that the presence of options may foster innovations among actors in the sector and consequently expand access to care by many.
Promote public buy-in for health insurance
Advocacy and awareness creation among the masses are also critical, and especially on the need for Kenyans to enroll in government schemes such as NHIF. As cited by Mr. Mwangi, the pay roll-based system ensures that employees participate. However, there needs to be advocacy among the unemployed and those in the informal sector so they can see the benefit of contributing to this healthcare pool of resources.
With regard to the policy framework, the Members of Parliament indicated that the Amendments to the Kenya Health Bill will be tabled in The House soon. Some of the amendments include the key issues on achievement of UHC discussed at the forum.
Judging from the discussions, Kenya has an excellent opportunity to achieve universal health care if the essential actions are taken. Besides government budgetary allocations and contributions by the private sector, good governance and advocacy will ensure every Kenyan has access to health services without being plunged into poverty.
The dialogue was hosted by AFIDEP’s Evidence for Development (EVI4DEV) programme which spearheaded the formation of the Parliamentary Caucus on Evidence-Informed Decision-Making (PC-EIDM). As highlighted by the Chair of the Caucus Hon. Susan Musyoka (MP, Machakos County), the main goal of the Caucus is to ensure that evidence becomes central to decision-making in parliament. This will ensure they make proper budgetary allocations and enhance accountability, which will bolster the country’s development.
Related Posts